July 29, 2013
Dr. Buford’s patients often ask about the scars from breast augmentation surgery. They pose many questions: Just how big will the incisions be? Will the resulting scars be thick or unsightly? And where are the incisions usually positioned? Today we will look at his approach for avoiding scars on the breasts and also review the pros and cons of various incision sites.
Caring for Your Scar
Scars are unavoidable with most surgeries, but their appearance can be greatly minimized when a skilled Plastic Surgeon performs the surgery and post-surgical instructions are followed. Scar care is an important part of any cosmetic procedure. Dr. Buford uses a multi-stage plan for reducing scars after breast augmentation:
- In the first week following surgery, dressings cover the incisions.
- In the second week, surgi-strips are used to hold the incision closed and reduce strain on the site while healing continues.
- After the surgi-strips come off, a special micro-pore tape is used to cover and support the scars for the next several months as they continue to heal. The latex-free, paper “scar tape” helps flatten the incisions and reduces the chances that they might widen as they heal.
Dr. Buford also uses Skin Medica’s Scar Recovery Gel for all of his surgical patients. This amazing product optimizes the scar outcome and is dramatically more effective than any over-the-counter product such as Mederma. One of the active ingredients in Scar Recovery Gel is centella asiatica, also known as gotu kola; this herb is full of vitamins and minerals, and also stimulates collagen production and reduces inflammation. Studies have shown that Scar Recovery Gel offers impressive improvement in the long-term appearance of any scar.
Planning the Incision Location
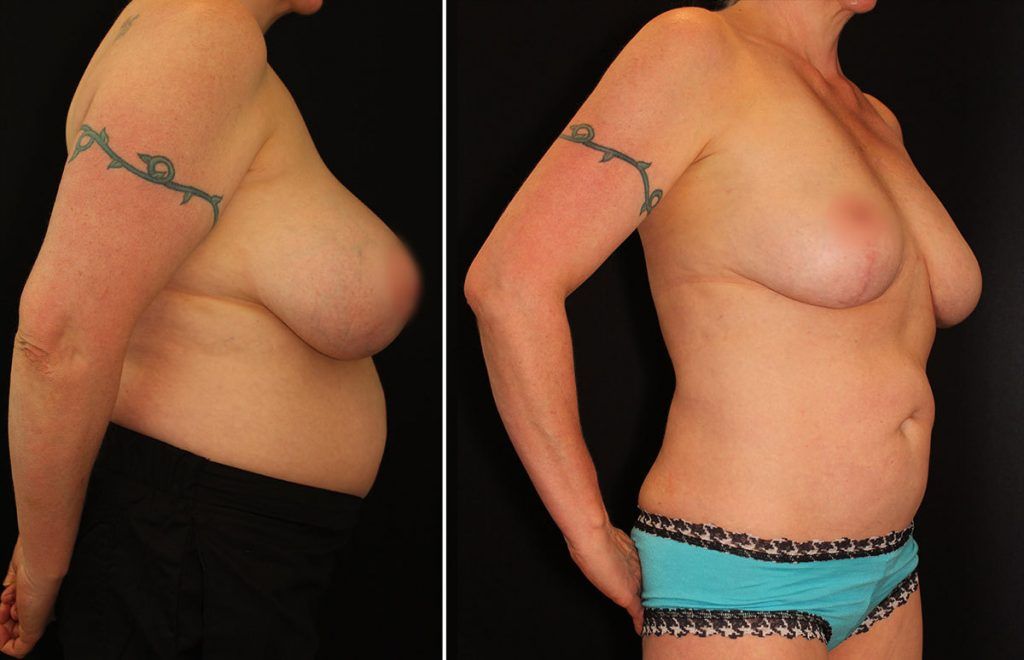
Now let’s look at incision placement for breast augmentation, starting first with Dr. Buford’s preferred method. The spot where the underside of the breast meets the chest wall is called the inframammary fold. This boundary offers a natural hiding place for the scar and the implants can be best positioned from this angle, allowing the surgeon to have excellent visibility when he is performing the augmentation. Any resulting scars will be very well hidden in this site. An underwire bra should not be worn during the recovery time, though, because it might irritate the incisions.
Many people don’t realize that the incision for a breast implant is sometimes made under the arm, in the axillary (armpit) area. This incision point may offer advantages for any woman who plans on breastfeeding sometime in the future, as it completely avoids the nerves and milk ducts. However, larger silicone gel implants (over 350cc) can be difficult to place from this site, and if revision surgery were to be necessary later, the new incision would have to be made at one of the other location options.
A peri-areolar incision follows the natural demarcation between the nipple and the breast itself. There is a slightly higher risk of losing nipple sensation with this approach and of the three incision options, a peri-areolar scar is on the most noticeable portion of the breast. The ability to breastfeed may be affected because the milk ducts may be compromised by the surgery.
Of course, each person heals differently and results cannot be guaranteed, but careful planning and diligent post-op care can greatly reduce the appearance of scars from breast augmentation, no matter which incision site is chosen. Dr. Buford takes great care to minimize all scarring from surgery; he even offers complimentary laser treatments to his breast augmentation patients if the conditions are appropriate. He is happy to discuss all the options for breast augmentation during a consultation.